Healthy knees are key to keeping our bodies in motion. From everyday walking or simply getting out of bed to intense athletic feats, our knee joints allow our legs to move in all the ways we need them to. For that reason, in case of a knee injury or another condition, it’s critical to get the right kinds of treatment so you’re slowed down as little as possible.
As your local physical therapy experts, JAG PT can help you rehabilitate a knee condition in the most effective way after you’ve consulted your physician. We’re well-versed in all of the ailments that can cause knee pain, stiffness, and other symptoms, and by consulting with our skilled physical therapists, you’ll benefit from a custom treatment plan that works best for your life.
Common Knee Injuries
Read more below about conditions that impair proper knee function for millions of people, or book your JAG PT appointment today and let us help you get your knees back to a pain-free range of motion.
Is Physical Therapy Good for Knee Pain?
Some forms of physical therapy are ideal long-term treatments for knee pain. Various methods, from orthopedic physical therapy to manual therapy, can actually provide immediate symptom relief, while also increasing strength and flexibility over time in order to improve knee function as a whole. At JAG PT, we also offer injury prevention services to make sure your knees’ condition is not worsened through later damage.
What Causes Pain in the Knee?
We think of the knee as just one bone – the patella, or kneecap. But the knee joint actually consists of four different bones – besides the patella, the femur, tibia, and fibula meet at this joint. The knee is also served by a number of ligaments, is surrounded by the hamstring and quadriceps muscles, and is supported by a crescent-shaped piece of cartilage called the meniscus. Damage to any of these parts, whether due to overuse, a fall, sudden blow, or other traumatic injury, or from inflammation or disease, can lead to pain that’s felt in the entire knee area.

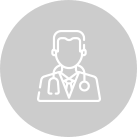
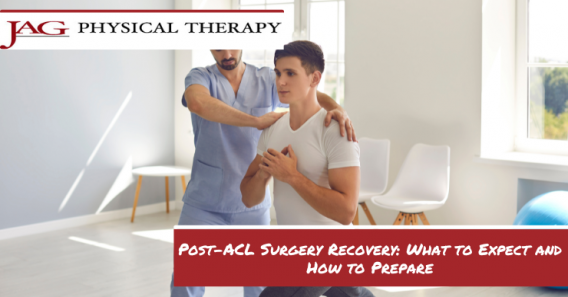
Physical Therapy Before and After Knee Surgery
Many surgeries on the knee are serious procedures which require a lot of recovery, even with advances in arthroscopic medicine. If you’re scheduled to have an operation on your knee – whether it’s surgery to repair a torn ACL, PLC reconstruction, a knee replacement, or something else – your physicians and surgical team will usually recommend you receive physical therapy both before and after you have your procedure. At JAG PT, our pre- and post-operative therapies focus on maintaining flexibility, joint stability, and reduced inflammation – all things that will lower your chances of complications and make your recovery go faster.
Knee Injury Signs and Symptoms
The symptoms of knee injury can include dull to sharp pain which can be immediate or arise later, inflammation, tenderness, and severely reduced mobility. Among the most common knee conditions are –
The anterior cruciate ligament, or ACL, maintains rotational stability in the knee joint. Sprains and tears to the ACL are some of the most often-seen knee injuries – 100,000 people tear their ACL yearly in the US alone. Usually caused by a sudden stop or change in direction when running or jumping, a torn ACL can result in a popping sensation followed by severe pain, swelling, and a sensation of instability in the leg.
The meniscus, a band of cartilage within the knee, can be torn seemingly at random when walking, standing up or sitting down, or squatting. Meniscus injuries can result in pain directly along the joint line and an inability to straighten the leg. They’re also particularly difficult to heal, because part of the meniscus is not served by any blood vessels and thus can’t receive the nutrients the body would otherwise send during the recovery process.
In cases of chondromalacia patellae, the underside of the kneecap becomes inflamed and the cartilage of the knee softens as a result (“chondromalacia” comes from the ancient Greek for “cartilage” and “softness”). Closely related to patellofemoral pain syndrome, chondromalacia patellae is usually caused by chronic friction between the patella and the femur. The change in texture of the cartilage can make anything rubbing against it very painful, which means movement of the knee becomes difficult.
Osgood-Schlatter disease is inflammation in one of the patellar ligaments. Its characteristic sign is a raised, painful bump below the knee. The resultant pain worsens when active and only improves over a period of time.
Osteochondritis dissecans is so called because it can cause dissection, or fragmentation, of both the cartilage and bone of the knee. Caused by a lack of blood supply and repetitive strain to the joint, one of the most serious symptoms is movement of the bone and cartilage fragments in the space of the knee, which can cause pain, blockage, and increasing damage over time.
Physical Therapy Methods in NY, NJ, and PA
At JAG Physical Therapy, we’ll consult with you and use our deep clinical knowledge to determine, together, what PT treatments are right for your knee injury. We may employ gait analysis through our sports medicine program, aquatic therapy, Graston technique, and more methods as necessary.
RELATED BLOGS & VIDEOS
See a Physical Therapist to Start Your Knee Injury Recovery
Given the importance of healthy knees, you should not procrastinate treating a knee injury. Find your nearest JAG PT location or book an appointment with us today.